Managing Psychosis: Effective Treatment Methods
Sep 05, 2024 By Martina Wlison
Treating patients with psychosis requires a nuanced approach that goes beyond medication alone. Psychosis, a condition marked by distorted thoughts, perceptions, and emotions, can severely impact an individual's life. For caregivers, medical professionals, and loved ones, knowing how to handle such situations is crucial for ensuring the patients well-being and recovery.
This article explores key strategies that are central to the effective treatment of psychosis, focusing on holistic care that integrates medication, therapy, and long-term support systems. By better understanding these approaches, we can provide more comprehensive care to those experiencing psychotic episodes, helping them regain stability and live fulfilling lives.
Proven Strategies to Treat Patients with Psychosis
Treating psychosis involves a combination of approaches that address both the symptoms and the underlying causes. The strategies below are based on evidence-based practices and have been shown to be effective in managing psychosis.
Medication Management: The Foundation of Treatment
Medications, especially antipsychotics, are often the first line of defense when treating psychosis. These help control symptoms such as hallucinations, delusions, and disorganized thinking. However, successful medication management goes beyond simply prescribing the right ones. It involves monitoring side effects, adjusting doses, and ensuring long-term compliance.

The challenge lies in finding the right balance. Some patients may experience significant side effects, like weight gain or drowsiness, which can lead them to stop taking their medications. A patient-centered approach that involves regular check-ins and adjustments is critical. Doctors often start with lower doses and increase gradually, allowing the patients body to adjust. Involving patients in these discussions helps build trust and encourages adherence to the treatment plan.
For many patients, a combination of newer antipsychotic drugs (like aripiprazole or risperidone) with older ones (like haloperidol) works well, depending on the specific symptoms. The goal is to find a regimen that minimizes symptoms while reducing side effects, ensuring the patient remains stable in the long term.
Cognitive Behavioral Therapy (CBT): Shaping Thought Patterns
While medication is essential, it doesnt address the psychological aspects of psychosis. Cognitive Behavioral Therapy (CBT) plays a crucial role in helping patients understand and manage their condition. CBT focuses on identifying and challenging distorted thinking patterns, making it especially effective for patients experiencing delusions and hallucinations.
Therapists work with patients to explore the underlying beliefs driving their symptoms. For instance, if a patient believes they are being watched, a CBT therapist would help them critically examine the evidence supporting this belief. Over time, the patient learns techniques to manage and reduce the impact of these thoughts.
CBT sessions are highly individualized and may also include techniques like exposure therapy, mindfulness, and relaxation exercises. When combined with medication, CBT offers a more holistic approach to treating psychosis. It not only reduces symptoms but also empowers patients by equipping them with tools to manage future episodes.
Family Support and Psychoeducation: Strengthening the Care Network
The role of family in the treatment of psychosis is often underestimated. Family members are usually the first to notice early warning signs and can play a significant role in a patients recovery. Psychoeducation programs are designed to educate families about the nature of psychosis, helping them understand what their loved one is going through and how to support them effectively.
A well-informed family is better equipped to handle relapses, understand the importance of medication adherence, and create a supportive environment at home. These programs often involve counseling sessions that teach communication skills, conflict resolution, and stress management techniques. Additionally, they help reduce the stigma and feelings of isolation often experienced by both the patient and their family.
Moreover, involving family members in therapy sessions can improve outcomes. Therapists might facilitate group discussions where both the patient and their family express their concerns, allowing everyone to feel heard and supported. This collaborative approach ensures that patients receive consistent care, both in clinical settings and at home.
Social Skills Training: Enhancing Daily Functioning
Psychosis often disrupts a persons ability to interact socially, leading to isolation and difficulties in daily functioning. Social skills training is a targeted intervention designed to rebuild these essential abilities. Patients are guided through practical exercises that improve communication, conflict resolution, and problem-solving skills.

For many with psychosis, social interactions become a source of anxiety and confusion. Social skills training breaks down these interactions into manageable steps. Patients practice scenarios like making small talk, resolving disagreements, or navigating public spaces. Role-playing exercises help them gain confidence in a safe and controlled environment.
Improving social skills also helps patients reintegrate into their communities, whether that means returning to work, attending school, or participating in social activities. The training often includes job readiness programs and educational support, making it easier for patients to rebuild their lives. By addressing the social and occupational aspects of recovery, social skills training ensures that patients regain not just mental stability but also a sense of purpose and belonging.
Early Intervention and Long-Term Follow-Up: Sustaining Recovery
Psychosis often first appears in young adults, making early intervention critical. The sooner treatment begins, the better the long-term outcomes. Early intervention services focus on identifying psychosis in its initial stages and providing immediate care. These programs are comprehensive, often combining medication, therapy, family support, and social services.
The key is to act quickly. Delayed treatment can lead to a longer duration of untreated psychosis (DUP), which is associated with worse outcomes. By catching the symptoms early, clinicians can prevent the condition from becoming more severe, helping patients maintain a higher level of functioning. Specialized early intervention teams often work with schools, universities, and community organizations to identify at-risk individuals.
However, early intervention is just the start. Sustaining recovery requires consistent follow-up care. Patients with psychosis benefit from ongoing monitoring even after their symptoms have stabilized. This includes regular check-ins with mental health professionals, medication reviews, and therapy sessions. Long-term support reduces the risk of relapse and ensures that any emerging issues are addressed promptly.
Conclusion
Treating patients with psychosis is a multifaceted process that requires more than just clinical expertise; it demands compassion, patience, and a deep understanding of the individuals needs. The combination of medication, therapy, family involvement, and social support forms a comprehensive framework for managing this complex condition.
By focusing on both the immediate and long-term aspects of care, we can help individuals with psychosis lead more stable and fulfilling lives. As awareness and understanding of psychosis grow, so too will our ability to offer better, more effective treatment options for those who need it most.
Understanding How OCD Medication Affects Your Personality

Techniques to Maintain and Improve Your Posture as You Grow Older
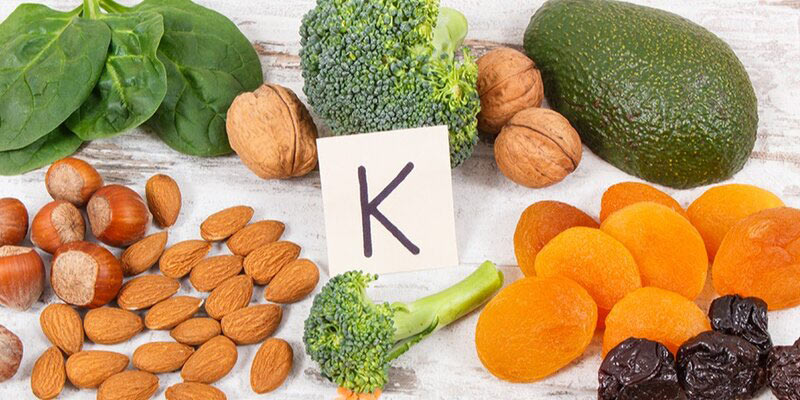
Vitamin K - A Key Player in Health

Can AI-Supported Mammogram Screening Really Help With Detection?

6 easy bowl recipes for a wholesome and nutritious dinner

How to Spot a Magnesium Deficiency: 7 Key Signs
Managing Psychosis: Effective Treatment Methods


